SARS-CoV-2: mucho más que un virus respiratorio
Resumen
Fundamento: el virus SARS-CoV-2 es responsable de la segunda pandemia del siglo XXI. Desde su aparición en China a finales de 2019, se asocia a neumonía y considera como un virus respiratorio más. Sin embargo, durante su diseminación global demuestra su capacidad para producir daño a otros órganos con manifestaciones clínicas nunca antes descritas para otros virus respiratorios.
Objetivo: describir la evidencia científica que respalde el daño extrapulmonar directo producido por el virus SARS-CoV-2 en etapas tardías de la infección, que apoyan su naturaleza bifásica y distinta frente a otros virus respiratorios.
Métodos: se realizó una búsqueda de artículos referente al tema en las bases de datos MEDLINE accedido desde PubMed, SciELO y LILACS. También se tuvieron en cuenta artículos publicados en los repositorios de preimpresión como medRxiv, BioRxiv. Mediante el gestor de búsqueda y administrador de referencias Mendeley, se eliminaron los duplicados y aquellos que no se ajustaban al objetivo del estudio, se seleccionaron 63 artículos para la revisión.
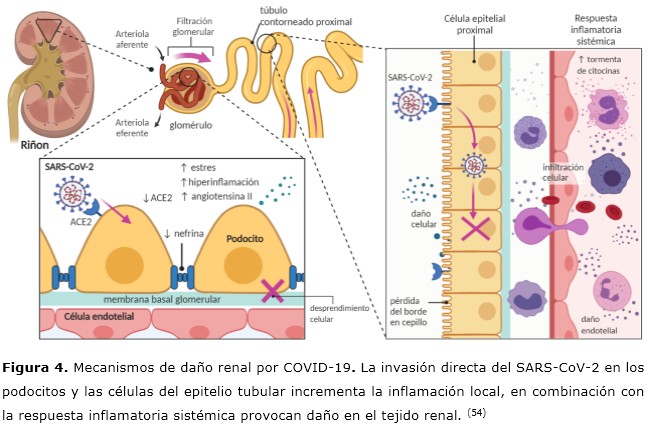
Resultados: la evidencia sugiere que el SARS-CoV-2 tiene tropismo no solo limitado a las vías respiratorias. La progresión clínica de la COVID-19 presenta un curso bifásico, con manifestaciones de tipo gripal en la primera fase y episodios postagudos y persistentes en la fase tardía, ocasionados por el daño directo al sistema nervioso central, cardiovascular, endocrino y renal.
Conclusiones: la infección por SARS-CoV-2 no debe considerarse solo como una infección aguda y circunscrita a las vías respiratorias.
DeCS: VIRUS DEL SRAS/patogenicidad; INFECCIONES POR CORONAVIRUS/transmisión; INFECCIONES DEL SISTEMA RESPIRATORIO/prevención & control; TROPISMO VIRAL/fisiología; REPLICACIÓN VIRAL.
Palabras clave
Referencias
World Health Organization. Timeline: WHO’s COVID-19 response [Internet]. Ginebra:WHO; 2020 [citado 22 Feb 2021]. Disponible en: https://bit.ly/3j1aOKF
Zheng KI, Feng G, Liu WY, Targher G, Byrne CD, Zheng MH. Extrapulmonary complications of COVID‐19: A multisystem disease? J Med Virol [Internet]. 2021 [citado 22 Feb 2021];93(1):323-335. Disponible en: https://doi.org/10.1002/jmv.26294
Yen CY, Wu WT, Chang CY, Wong YC, Lai CC, Chan YJ, et al. Viral etiologies of acute respiratory tract infections among hospitalized children-A comparison between single and multiple viral infections. J Microbiol Immunol Infect [Internet]. 2019 [citado 22 Feb 2021];52(6):902–10. Disponible en: https://doi.org/10.1016/j.jmii.2019.08.013
Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S. Transmission routes of respiratory viruses among humans. Curr Opin Virol [Internet]. 2018 [citado 22 Feb 2021];28:142–51. Disponible en: https://dx.doi.org/10.1016%2Fj.coviro.2018.01.001
Sellers SA, Hagan RS, Hayden FG, Fischer WA. The hidden burden of influenza: A review of the extra-pulmonary complications of influenza infection. Influenza Other Respi Viruses [Internet]. 2017 [citado 22 Feb 2021];11(5):372–93. Disponible en: https://doi.org/10.1111/irv.12470
Lowry K, Woodman A, Cook J, Evans DJ. Recombination in Enteroviruses Is a Biphasic Replicative Process Involving the Generation of Greater-than Genome Length Imprecise Intermediates. PLoS Pathog [Internet]. 2014 [citado 22 Feb 2021];10(6):e1004191. Disponible en: https://dx.doi.org/10.1371%2Fjournal.ppat.1004191
Charlton CL, Babady E, Ginocchio CC, Hatchette TF, Jerris RC, Li Y, et al. Practical Guidance for Clinical Microbiology Laboratories: Viruses Causing Acute Respiratory Tract Infections. Clin Microbiol Rev [Internet]. 2018;32(1): Disponible en: https://dx.doi.org/10.1128%2FCMR.00042-18
Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med [Internet]. 2018 [citado 22 Feb 2021];378(4):345–53. Disponible en: https://doi.org/10.1056/nejmoa1702090
Mejuto Fernández R. Complicaciones neurológicas asociadas al virus de la gripe [Tesis]. Cantabria: Universidad de Cantabria; 2015 [citado 22 Feb 2021]. Disponible en: https://repositorio.unican.es/xmlui/handle/10902/6795
Ing AJ, Cocks C, Green JP. COVID-19: in the footsteps of Ernest Shackleton. Thorax [Internet]. 2020 [citado 22 Feb 2021];75(8):693–4. Disponible en: http://dx.doi.org/10.1136/thoraxjnl-2020-215091
Sánchez-Oro R, Torres Nuez J, Martínez-Sanz G. La radiología en el diagnóstico de la neumonía por SARS-CoV-2 (COVID-19). Med Clin (Barc) [Internet]. 2020 [citado 22 Feb 2021];155(1):36-40. Disponible en: https://dx.doi.org/10.1016%2Fj.medcli.2020.03.004
Ooi EE, Low JG. Asymptomatic SARS-CoV-2 infection. Lancet Infect Dis [Internet]. 2020 [citado 22 Feb 2021];20(9):996–8. Disponible en: https://doi.org/10.1016/S1473-3099(20)30460-6
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus Disease 2019-COVID-19. Clin Microbiol Rev [Internet]. 2020 [citado 22 Feb 2021];33(4):[aprox. 14 p.]. Disponible en: https://cmr.asm.org/content/cmr/33/4/e00028-20.full.pdf https://doi.org/10.1128/CMR.00028-20
Hu B, Huang S, Yin L. The cytokine storm and COVID‐19. J Med Virol [Internet]. 2021 [citado 22 Feb 2021];93(1):250-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7361342/pdf/JMV-9999-na.pdf https://doi.org/10.1002/jmv.26232
Gupta A, Madhavan M V, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med [Internet]. 2020 [citado 22 Feb 2021];26(7):1017–32. Disponible en: https://doi.org/10.1038/s41591-020-0968-3
Wang K, Chen W, Zhou YS, Lian JQ, Zhang Z, Du P, et al. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv [Internet]. 2020 [citado 22 Feb 2021];3(14):988345. Disponible en: https://www.biorxiv.org/content/10.1101/2020.03.14.988345v1.full.pdf
Radzikowska U, Ding M, Tan G, Zhakparov D, Peng Y, Wawrzyniak P, et al. Distribution of ACE2, CD147, CD26, and other SARS‐CoV‐2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID‐19 risk factors. Allergy [Internet]. 2020 [citado 22 Feb 2021];75(11):2829-2845. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7300910/pdf/ALL-9999-na.pdf
doi: 10.1111/all.14429
Cantuti Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science [Internet]. 2020 [citado 22 Feb 2021];370(6518):856-860. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7857391/pdf/370_856.pdf
doi: 10.1126/science.abd2985
Jamal N, Whittier S, Carter RC, Zachariah P. Biphasic Variation Over Time in Presenting Features of Patients With COVID-19. Pediatrics [Internet]. 2020 [citado 22 Feb 2021];146(5):[aprox. 5 p.]. Disponible en: https://pediatrics.aappublications.org/content/pediatrics/146/5/e2020014902.full.pdf https://doi.org/10.1542/peds.2020-014902
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using Open SAFELY. Nature [Internet]. 2020 [citado 22 Feb 2021];584(7821):430–6. Disponible en: https://doi.org/10.1038/s41586-020-2521-4
Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19. JAMA [Internet]. 2020 [citado 22 Feb 2021];324(6):603. Disponible en: https://doi.org/10.1001/jama.2020.12603
Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ [Internet]. 2020 [citado 22 Feb 2021];370:m3026. Disponible en: https://doi.org/10.1136/bmj.m3026
Gallagher J. Coronavirus: qué es la COVID-19 crónica y por qué a algunos les cuesta tanto recuperarse. BBC News [Internet]. 2020 [citado 22 Feb 2021]. Disponible en: https://www.bbc.com/mundo/noticias-54434271
Memoli MJ, Han A, Walters KA, Czajkowski L, Reed S, Athota R, et al. Influenza A Reinfection in Sequential Human Challenge: Implications for Protective Immunity and Universal Vaccine Development. Clin Infect Dis [Internet]. 2020 [citado 22 Feb 2021];70(5):748–53. Disponible en: https://doi.org/10.1093/cid/ciz281
Heinonen S, Jartti T, Garcia C, Oliva S, Smitherman C, Anguiano E, et al. Rhinovirus Detection in Symptomatic and Asymptomatic Children: Value of Host Transcriptome Analysis. Am J Respir Crit Care Med [Internet]. 2016 [citado 22 Feb 2021];193(7):772-82. Disponible en: https://dx.doi.org/10.1164%2Frccm.201504-0749OC
Tillett RL, Sevinsky JR, Hartley PD, Kerwin H, Crawford N, Gorzalski A, et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis [Internet]. 2021 [citado 22 Feb 2021];21(1):52-58. Disponible en: https://doi.org/10.1016/S1473-3099(20)30764-7
Zlateva KT, de Vries JJC, Coenjaerts FEJ, van Loon AM, Verheij T, Little P, et al. Prolonged shedding of rhinovirus and re-infection in adults with respiratory tract illness. Eur Respir J [Internet]. 2014 [citado 22 Feb 2021];44(1):169-77. Disponible en: https://doi.org/10.1183/09031936.00172113
Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and Ageusia: Common Findings in COVID‐19 Patients. Laryngoscope [Internet]. 2020 [citado 22 Feb 2021];130(7):1787–1787. Disponible en: https://dx.doi.org/10.1002%2Flary.28692
Lechien JR, Chiesa Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Oto Rhino Laryngology [Internet]. 2020 [citado 22 Feb 2021];277(8):2251–61. Disponible en: https://dx.doi.org/10.1007%2Fs00405-020-05965-1
Vaira LA, Hopkins C, Petrocelli M, Lechien JR, Soma D, Giovanditto F, et al. Do olfactory and gustatory psychophysical scores have prognostic value in COVID-19 patients? A prospective study of 106 patients. J Otolaryngol Head Neck Surg [Internet]. 2020 [citado 22 Feb 2021];49(1):56. Disponible en: https://dx.doi.org/10.1186%2Fs40463-020-00449-y
Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis [Internet]. 2020 [citado 22 Feb 2021];94:55-8. Disponible en: https://dx.doi.org/10.1016%2Fj.ijid.2020.03.062
Sharifian Dorche M, Huot P, Osherov M, Wen D, Saveriano A, Giacomini PS, et al. Neurological complications of coronavirus infection; a comparative review and lessons learned during the COVID-19 pandemic. J Neurol Sci [Internet]. 2020 [citado 22 Feb 2021];417:[aprox. 15 p.]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7413162/pdf/main.pdf https://dx.doi.org/10.1016%2Fj.jns.2020.117085
Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol [Internet]. 2020 [citado 22 Feb 2021];19(9):767–83. Disponible en: https://dx.doi.org/10.1016%2FS1474-4422(20)30221-0
Najjar S, Najjar A, Chong DJ, Pramanik BK, Kirsch C, Kuzniecky RI, et al. Central nervous system complications associated with SARS-CoV-2 infection: integrative concepts of pathophysiology and case reports. J Neuroinflammation [Internet]. 2020 [citado 22 Feb 2021];17(1):231. Disponible en: https://dx.doi.org/10.1186%2Fs12974-020-01896-0
Holmes JL, Brake S, Docherty M, Lilford R, Watson S. Emergency ambulance services for heart attack and stroke during UK’s COVID-19 lockdown. Lancet [Internet]. 2020 [citado 22 Feb 2021];395(10237):e93–4. Disponible en: https://doi.org/10.1016/S0140-6736(20)31031-X
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med [Internet]. 2020 [citado 22 Feb 2021];8(4):420–2. Disponible en: https://doi.org/10.1016/S2213-2600(20)30076-X
Dolhnikoff M, Ferreira Ferranti J, de Almeida Monteiro RA, Duarte-Neto AN, Soares Gomes-Gouvêa M, ViuDegaspare N, et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc Heal [Internet]. 2020 [citado 22 Feb 2021];4(10):790–4. Disponible en: https://doi.org/10.1016/S2352-4642(20)30257-1
Pirzada A, Mokhtar AT, Moeller AD. COVID-19 and Myocarditis: What Do We Know So Far? CJC Open [Internet]. 2020 [citado 22 Feb 2021];2(4):278-85. Disponible en: https://doi.org/10.1016/j.cjco.2020.05.005
Buja LM, Wolf DA, Zhao B, Akkanti B, McDonald M, Lelenwa L, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): Report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol [Internet]. 2020 [citado 22 Feb 2021];48:107233. Disponible en: https://doi.org/10.1016/j.carpath.2020.107233
Bernal Torres W, Herrera Escandón Á, Hurtado Rivera M, Plata Mosquera CA. COVID-19 fulminant myocarditis: a case report. Eur Hear J Case Reports [Internet]. 2020 [citado 22 Feb 2021];4(FI1):1-6. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7454494/pdf/ytaa212.pdf https://doi.org/10.1093/ehjcr/ytaa212
Iacobellis G, Penaherrera CA, Bermudez LE, Bernal Mizrachi E. Admission hyperglycemia and radiological findings of SARS-CoV2 in patients with and without diabetes. Diabetes Res Clin Pract [Internet]. 2020 [citado 22 Feb 2021];164:108185. Disponible en: https://dx.doi.org/10.1016%2Fj.diabres.2020.108185
Bode B, Garrett V, Messler J, McFarland R, Crowe J, Booth R, et al. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J Diabetes SciTechnol [Internet]. 2020 [citado 22 Feb 2021];14(4):813–21. Disponible en: https://doi.org/10.1177%2F1932296820924469
Marik PE, Bellomo R. Stress hyperglycemia: an essential survival response! Crit Care [Internet]. 2013 [citado 22 Feb 2021];17(2):305. Disponible en: https://doi.org/10.1186/cc12514
Wei L, Sun S, Xu C, Zhang J, Xu Y, Zhu H, et al. Pathology of the thyroid in severe acute respiratory syndrome. Hum Pathol [Internet]. 2007 [citado 22 Feb 2021];38(1):95–102. Disponible en: https://doi.org/10.1016/j.humpath.2006.06.011
Yao XH, TY L. Histopathological study of new coronavirus pneumonia (COVID-19) in three patients. Chinese J Pathol [Internet]. 2020 [citado 22 Feb 2021];49. Disponible en: https://bit.ly/348pOCc
Vishvkarma R, Rajender S. Could SARS‐CoV‐2 affect male fertility? Andrologia [Internet]. 2020 [citado 22 Feb 2021];52(9). Disponible en: https://doi.org/10.1111/and.13712
Zupin L, Pascolo L, Zito G, Ricci G, Crovella S. SARS-CoV-2 and the next generations: which impact on reproductive tissues? J Assist Reprod Genet [Internet]. 2020 [citado 22 Feb 2021];37(10):2399–403. Disponible en: https://doi.org/10.1007/s10815-020-01917-0
Bunders MJ, Altfeld M. Implications of Sex Differences in Immunity for SARS-CoV-2 Pathogenesis and Design of Therapeutic Interventions. Immunity [Internet]. 2020 [citado 22 Feb 2021];53(3):487-95. Disponible en: https://doi.org/10.1016/j.immuni.2020.08.003
Li M-Y, Li L, Zhang Y, Wang X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty [Internet]. 2020 [citado 22 Feb 2021];9(1):45. Disponible en: https://doi.org/10.1186/s40249-020-00662-x
Ding Y, He L, Zhang Q, Huang Z, Che X, Hou J, et al. Organ distribution of severe acute respiratory syndrome(SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol [Internet]. 2004 [citado 22 Feb 2021];203(2):622-30. Disponible en: https://doi.org/10.1002/path.1560
Zinserling VA, Semenova NY, Markov AG, Rybalchenko O V, Wang J, Rodionov RN, et al. Inflammatory Cell Infiltration of Adrenals in COVID-19. Horm Metab Res [Internet]. 2020 [citado 22 Feb 2021];52(09):639-41. Disponible en: https://doi.org/10.1055/a-1191-8094
Su H, Yang M, Wan C, Yi L-X, Tang F, Zhu H-Y, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int [Internet]. 2020 [citado 22 Feb 2021];98(1):219–27. Disponible en: https://doi.org/10.1016/j.kint.2020.04.003
Schurink B, Roos E, Radonic T, Barbe E, Bouman CSC, de Boer HH, et al. Viral presence and immunopathology in patients with lethal COVID-19: a prospective autopsy cohort study. Lancet Microbe [Internet]. 2020 [citado 22 Feb 2021];1(7):[aprox. 8 p.]. Disponible en: https://doi.org/10.1016/S2666-5247(20)30144-0
Martinez-Rojas MA, Vega-Vega O, Bobadilla NA. Is the kidney a target of SARS-CoV-2? Am J Physiol Physiol [Internet]. 2020 [citado 22 Feb 2021];318(6):F1454–62. Disponible en: https://doi.org/10.1152/ajprenal.00160.2020
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA [Internet]. 2020 [citado 22 Feb 2021];323(18):1843-1844. Disponible en: https://doi.org/10.1001/jama.2020.3786
Yu F, Yan L, Wang N, Yang S, Wang L, Tang Y, et al. Quantitative Detection and Viral Load Analysis of SARS-CoV-2 in Infected Patients. Clin Infect Dis [Internet]. 2020 [citado 22 Feb 2021];71(15):793–8. Disponible en: https://doi.org/10.1093/cid/ciaa345
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature [Internet]. 2020 [citado 22 Feb 2021];581(7809):465–9. Disponible en: https://doi.org/10.1038/s41586-020-2196-x
Knoops K, Kikkert M, Worm SHE van den, Zevenhoven Dobbe JC, van der Meer Y, Koster AJ, et al. SARS-coronavirus replication is supported by a reticulovesicular network of modified endoplasmic reticulum. PLoSBiol [Internet]. 2008 [citado 22 Feb 2021];6(9):e226. Disponible en: https://doi.org/10.1371/journal.pbio.0060226
Baglivo M, Baronio M, Natalini G, Beccari T, Chiurazzi P, Fulcheri E, et al. Natural small molecules as inhibitors of coronavirus lipid-dependent attachment to host cells: a possible strategy for reducing SARS-COV-2 infectivity? Acta Biomed [Internet]. 2020 [citado 22 Feb 2021];91(1):161–4. Disponible en: https://dx.doi.org/10.23750%2Fabm.v91i1.9402
Tanida I, Fukasawa M, Ueno T, Kominami E, Wakita T, Hanada K. Knockdown of autophagy-related gene decreases the production of infectious Hepatitis C virus particles. Autophagy [Internet]. 2009 [citado 22 Feb 2021];5(7):937-45. Disponible en: https://doi.org/10.4161/auto.5.7.9243
Elrashdy F, Aljaddawi AA, Redwan EM, Uversky VN. On the potential role of exosomes in the COVID-19 reinfection/reactivation opportunity. J Biomol Struct Dyn [Internet]. 2020 [citado 22 Feb 2021];1-12. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7441802/pdf/TBSD_0_1790426.pdf https://dx.doi.org/10.1080%2F07391102.2020.1790426
Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun [Internet]. 2020 [citado 22 Feb 2021];11(1):1620. Disponible en: https://doi.org/10.1038/s41467-020-15562-9
Xia S, Liu M, Wang C, Xu W, Lan Q, Feng S, et al. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res [Internet]. 2020 [citado 22 Feb 2021];30(4):343–55. Disponible en: https://doi.org/10.1038/s41422-020-0305-x
Enlaces refback
- No hay ningún enlace refback.

Esta obra está bajo una licencia de Creative Commons Reconocimiento-NoComercial 4.0 Internacional.











 La Revista está: Certificada por el CITMA
La Revista está: Certificada por el CITMA Acreditados como: "Web de Interés Sanitario"
Acreditados como: "Web de Interés Sanitario"
